Imaging’s Role in Hospital Decision-Making
Medical imaging sits at the center of modern healthcare. Radiology is one of the few specialties that touches nearly every patient pathway—emergency admissions, surgical planning, oncology, orthopedics, cardiology, pediatrics, and even preventive health. In many cases, treatment decisions hinge almost entirely on what the images reveal.
Medical imaging has long been at the heart of modern diagnostics. Radiology alone touches nearly every patient pathway, and in many specialties, treatment decisions hinge almost entirely on what the images reveal. Yet despite this central role, imaging remains one of the most underleveraged assets in hospital operations. The problem isn’t the image itself — it’s how hospitals manage, share, and act on it. PACS changed the way hospitals store and retrieve studies, eliminating film archives and making results easier to access. Hospital management systems reorganized how admissions, orders, and clinical records are managed. But in many facilities, these systems continue to function separately. Imaging results are often stored in one system while patient data, lab values, and treatment notes are kept in another. This separation slows down reporting, forces staff to spend more time coordinating information, and limits the ability to use imaging data for broader goals such as quality improvement, population health planning, and precision medicine initiatives.
Enterprise Imaging Integration: From Departmental Tool to Hospital Resource
Hospitals are increasingly moving toward enterprise imaging integration — ensuring that imaging is not managed separately in the radiology department but is connected to the hospital’s central management system. When PACS is integrated with the HMS, studies and reports are available alongside patient records, laboratory results, and treatment plans.
This integration ensures that:
- Clinicians see the full patient picture at the point of care.
- Administrators gain better oversight of equipment use, reporting turnaround, and cost control.
- Health information teams maintain a consistent record across the organization, reducing duplication and errors.
Why Imaging Remains Underutilized
Although imaging sits at the center of nearly every clinical decision pathway, hospitals often fail to maximize its potential across the enterprise. The issue lies not with the technology of imaging itself, but with how it is managed and shared within the broader hospital ecosystem.
In many facilities, Picture Archiving and Communication Systems (PACS) and Hospital Management Systems (HMS) continue to function independently. PACS is optimized for storing and retrieving radiology images, while HMS is designed to manage patient admissions, orders, billing, and electronic health records. When these systems remain disconnected, imaging data sits in silos, accessible only to certain departments.
This separation creates several operational bottlenecks that administrators, clinicians, and nurses encounter every day:
- Fragmented patient records – A clinician reviewing an MRI may have to toggle between PACS for images and HMS for lab results or clinical notes, slowing down decision-making.
- Inefficient reporting workflows – Radiologists complete reports in PACS, but results may take time to reach physicians in other specialties, delaying treatment initiation.
- Duplicated investigations – Without consolidated access, the same patient may undergo unnecessary repeat scans because prior studies are not visible in the HMS.
- Limited oversight for administrators – Equipment utilization, turnaround times, and reporting efficiency are harder to monitor when imaging is managed separately from hospital operations.
In short, while imaging is indispensable to clinical care, its value is diminished when confined to a single department. Hospitals that fail to integrate PACS with HMS risk slower clinical pathways, higher operational costs, and missed opportunities for hospital-wide performance improvement.
The Opportunity: PACS and HMS Integration
The future of hospital efficiency lies in bringing imaging data out of departmental silos and embedding it within the hospital’s central information flow. By integrating PACS with HMS, hospitals transform imaging from a standalone tool into an enterprise-wide asset.
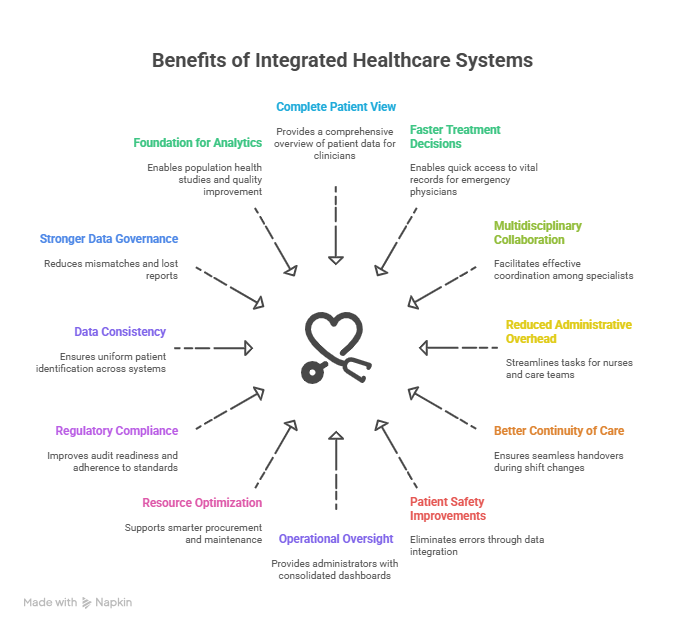
This integration ensures that imaging studies, radiology reports, and clinical data no longer exist in parallel systems but are unified into a single patient record. The benefits are not limited to radiology alone; every stakeholder in the hospital ecosystem gains measurable value.
For Clinicians
- Complete patient view at the point of care: A surgeon preparing for an operation can review lab values, prior admissions, and radiology studies on one screen, avoiding time-consuming cross-checks.
- Faster treatment decisions: Emergency physicians can immediately access both imaging reports and vital records, reducing delays in life-saving interventions.
- Multidisciplinary collaboration: Specialists in oncology, cardiology, and orthopedics can coordinate more effectively when imaging data is available in the same environment as lab tests and treatment plans.
For Nurses and Care Teams
- Reduced administrative overhead: Nurses no longer need to track down results from multiple systems before updating patient charts.
- Better continuity of care: Imaging findings are automatically reflected in the central record, enabling seamless handovers during shift changes.
- Patient safety improvements: Eliminating duplicate data entry and manual reporting reduces transcription errors.
For Hospital Administrators
- Operational oversight: Administrators gain consolidated dashboards showing imaging turnaround times, scanner utilization rates, and cost per study.
- Resource optimization: Insights into equipment usage support smarter procurement, maintenance scheduling, and workload balancing.
- Regulatory compliance: Centralized records improve audit readiness and adherence to global and local standards.
For Health Information Management Teams
- Data consistency: A single patient identifier ensures that imaging and clinical data are not duplicated across systems.
- Stronger data governance: Integrated workflows reduce mismatches, lost reports, and incomplete patient records.
- Foundation for analytics: When imaging is tied to hospital-wide data, it becomes a powerful resource for population health studies, quality improvement, and outcome tracking.
In essence, PACS–HMS integration elevates imaging from a departmental function to a hospital-wide strategic resource. It turns raw images into actionable intelligence—accelerating decision-making, improving collaboration, and optimizing both clinical and financial performance.
Key Benefits of Enterprise Imaging Intelligence
When hospitals succeed in pairing PACS with their HMS, imaging becomes more than just a diagnostic snapshot — it turns into a strategic lever for clinical care, operational efficiency, and financial stability. Below are the core benefits as experienced by different stakeholders inside a healthcare facility.
Clinical Decision-Making at the Point of Care
For physicians, every second counts, especially in critical care and emergency medicine. A fully integrated PACS–HMS environment means:
- One patient record, one source of truth: Physicians see imaging alongside lab reports, clinical notes, and past medical history without toggling between systems.
- Reduced delays in emergencies: In trauma or stroke cases, radiology reports can be reviewed directly from the HMS interface, allowing interventions like thrombolysis or surgery to be initiated faster.
- Support for multidisciplinary boards: Oncology tumor boards, orthopedic surgical teams, and cardiology case reviews all benefit from having images and reports presented in the same environment as treatment notes and laboratory results.
Nursing and Care Team Coordination
Nurses are the backbone of patient monitoring and continuity of care. Integration helps them by:
- Streamlining patient handovers: Imaging updates are automatically recorded in the central patient record, ensuring smooth communication between shifts.
- Avoiding duplication: Nurses no longer have to manually request or re-check imaging results from radiology, reducing administrative overhead.
- Safer medication administration: Imaging findings, such as the detection of renal impairment or pulmonary changes, are aligned with treatment notes, helping prevent inappropriate prescriptions.
Administrative Oversight and Resource Utilization
Hospital administrators face increasing pressure to balance cost control with service quality. PACS–HMS integration provides:
- Comprehensive dashboards: Turnaround times, modality utilization (CT, MRI, ultrasound), and reporting delays are visible in real time.
- Better asset management: Understanding scan volumes per modality aids in procurement planning, preventive maintenance scheduling, and workforce allocation.
- Benchmarking and compliance: Administrators can compare departmental KPIs, track adherence to turnaround standards, and meet reporting obligations set by national health authorities.
Health Information Management and Compliance
Health information teams are responsible for data integrity, coding, and compliance. Integrated imaging brings them:
- Data quality improvements: Linking images with hospital master patient indexes reduces duplicate entries and mismatched reports.
- Audit readiness: Imaging becomes part of the longitudinal patient record, simplifying compliance with and regional frameworks
- Foundation for analytics: Unified records make it easier to conduct hospital-wide reviews — for instance, evaluating whether imaging follow-ups are being completed as per clinical guidelines.
Financial Performance and Cost Control
Finance teams, often overlooked in IT integration, gain tangible benefits:
- Reduced unnecessary repeat scans: Integration prevents duplicate imaging orders, cutting direct costs.
- Improved billing accuracy: Imaging procedures are captured in the same system as patient encounters, reducing missed charges.
- Revenue insights: Hospitals can analyze revenue contributions from imaging services and evaluate ROI on expensive modalities.
Implementation Challenges and Best Practices
Bringing together PACS and HMS into a unified enterprise imaging environment is not without its hurdles. Many hospitals underestimate the scope of integration until they are mid-project, when technical, organizational, and compliance issues surface. Below are the most common challenges — along with practices that leading hospitals have adopted to overcome them.
Technical Challenges
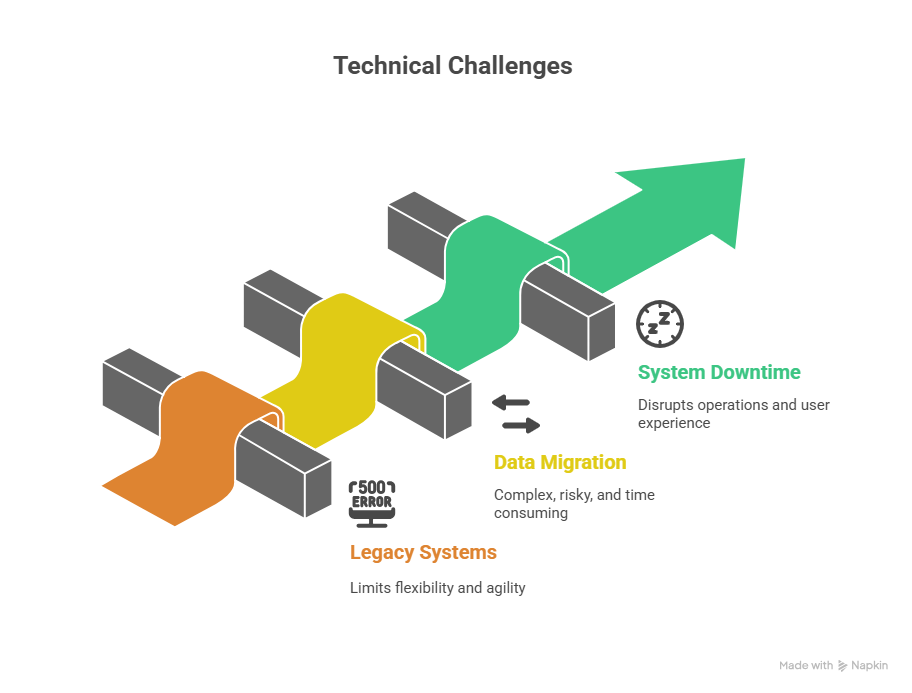
Legacy Systems and Vendor Lock-In
Many hospitals still rely on older PACS or siloed departmental systems. These platforms may not support modern interoperability standards such as DICOM or HL7 creating integration roadblocks.
Best Practice: Before embarking on integration, conduct a full system audit — cataloging PACS versions, HMS modules, interface engines, and networking capabilities. Hospitals that plan for phased modernization (rather than a big-bang replacement) reduce downtime and disruption.
Data Migration and Storage
Imaging archives can span decades, running into hundreds of terabytes. Migrating such volumes from standalone PACS to an enterprise storage layer is both costly and risky.
Best Practice: Prioritize migration by clinical relevance and usage frequency. Recent and frequently accessed studies should move first, while long-term archives may remain in a separate but searchable repository. A hybrid model ensures continuity while managing costs.
Downtime and System Performance
Even small integration missteps can lead to system lags, directly affecting clinical operations. For example, radiologists waiting for images to load or clinicians facing report delays.
Best Practice: Hospitals that succeed here always pilot-test integration in a controlled environment before rolling out facility-wide. Simulation labs where clinicians can test workflows under near-real conditions are invaluable.
Organizational Challenges
Change Management
Integrations often fail not because of technology, but because clinicians and staff resist new workflows. Radiology may be concerned about losing departmental autonomy, while nursing units may fear additional data-entry burdens.
Best Practice: Establish a cross-functional steering committee early, with representatives from radiology, IT, nursing, finance, and administration. Involving end-users in design decisions fosters adoption and avoids “IT-imposed” workflows.
Training and Adoption
New systems demand new habits. If staff aren’t adequately trained, they revert to old methods — printing reports, duplicating orders, or bypassing the HMS entirely.
Best Practice: Develop role-based training that reflects real-world use cases — for instance, how an ER physician retrieves a CT angiogram within the HMS, or how a nurse verifies an imaging report before administering treatment.
Compliance and Security Challenges

Data Privacy
Imaging data is among the most sensitive patient information. Breaches or unauthorized sharing can result in both reputational damage and legal penalties.
Best Practice: Adopt access-based restrictions with audit trails. Not every staff member should see full-resolution imaging; permissions must reflect clinical need-to-know.
Regulatory Alignment
Different regions impose distinct requirements —integrations must comply with data retention, transmission, and reporting standards.
Best Practice: Partner with certified intermediaries and compliance consultants during integration. Hospitals that align with regulators from the outset avoid costly retrofits later.
Financial and Operational Challenges
Budget Constraints
Enterprise imaging projects can strain hospital budgets, especially when competing with other infrastructure needs.
Best Practice: Develop a clear ROI model before starting. Quantify benefits in terms of reduced repeat scans, improved turnaround times, and billing capture. Hospitals that communicate the financial upside to boards and investors secure smoother funding approval.
Scalability and Future-Proofing
Hospitals are dynamic — expanding services, adding branches, onboarding new specialties. Systems that cannot scale quickly risk obsolescence.
Best Practice: Choose vendors and architectures that support modularity and cloud-readiness, so the integration grows with the hospital rather than holding it back.
The Road Ahead — Imaging as a Strategic Asset
Hospitals are no longer thinking of imaging as a departmental function. The emerging consensus is clear: when medical images are fully integrated into the hospital’s core information systems, they become a strategic enterprise asset. This shift has implications that extend well beyond radiology, influencing clinical outcomes, operational efficiency, financial sustainability, and even population health initiatives.
Imaging in Value-Based Care Models
Global healthcare is moving steadily toward value-based reimbursement, where outcomes and efficiency matter as much as volume. In this environment, imaging intelligence helps hospitals demonstrate:
- Reduced unnecessary scans by enabling better visibility of patient imaging histories across departments and branches.
- Faster care coordination, as physicians access images and reports directly within the HMS without delays or duplications.
- Improved clinical outcomes, supported by structured reporting and standardized image sharing.
Hospitals that integrate PACS and HMS position themselves to thrive under outcome-driven payment systems, avoiding penalties linked to duplication or delayed diagnoses.
Multi-Hospital Networks and Regional Collaboration
Healthcare delivery is increasingly networked. Many systems operate across multiple facilities, each with its own PACS or departmental workflows.
With enterprise imaging intelligence:
- A regional health system can access imaging across hospitals in real-time, improving patient transfers and referrals.
- Clinicians at tertiary centers can review scans from satellite facilities instantly, ensuring timely interventions.
- Administrators can track imaging utilization across the network, identifying inefficiencies and optimizing capacity.
This network-wide visibility supports strategic goals such as consolidation, resource-sharing, and equitable care delivery.
Telemedicine and Remote Collaboration
Telehealth is no longer an optional service; it is a cornerstone of modern patient care. Imaging plays a central role here, whether in teleradiology, remote second opinions, or virtual tumor boards. Without PACS–HMS integration, telemedicine workflows are fragmented, requiring separate logins, image viewers, and reporting systems.
Integrated enterprise imaging allows:
- Radiologists to report from any location with secure HMS access.
- Surgeons to review diagnostic scans remotely before making critical decisions.
- Multidisciplinary teams to collaborate on cases in virtual environments with imaging embedded into shared records.
This not only extends the reach of care but ensures clinical continuity regardless of where the patient is located.
Operational and Financial Intelligence
Hospitals that harness imaging as a strategic asset gain a new layer of business intelligence. For example:
- CFOs can monitor imaging utilization by department, aligning capacity with demand.
- Operations managers can track turnaround times and identify workflow bottlenecks.
- Quality officers can analyze imaging-linked adverse events or delays to improve safety.
These insights help healthcare leaders make data-backed decisions on staffing, equipment purchases, and service-line expansion.
Future Outlook
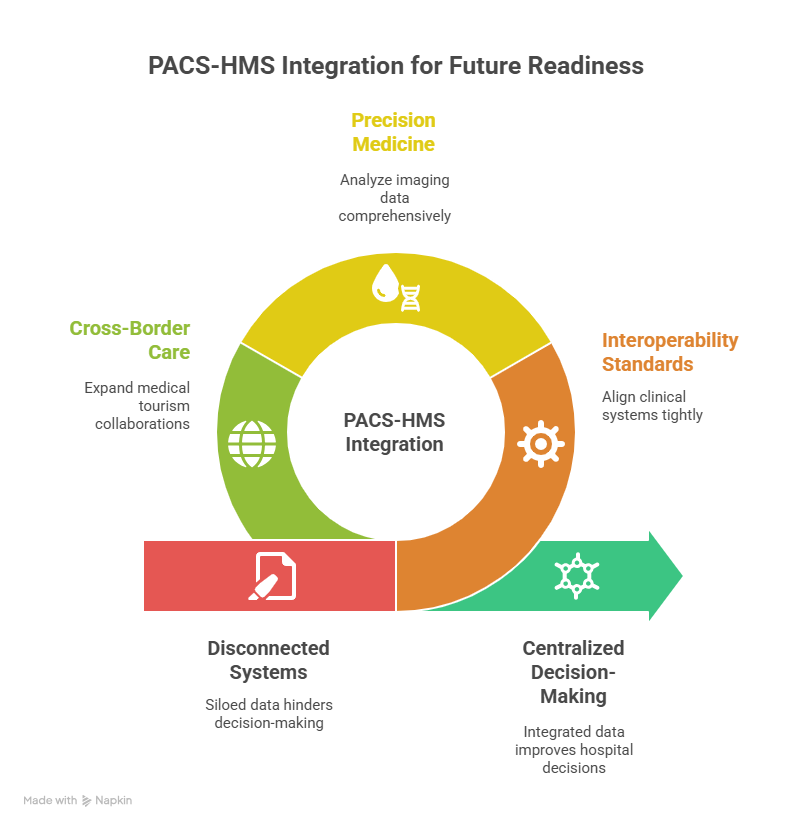
The trajectory is clear. Enterprise imaging intelligence will continue to mature, evolving into a central nervous system for hospital decision-making. Hospitals that embrace PACS–HMS integration today will be better prepared for:
- Next-generation interoperability standards that demand tighter clinical system alignment.
- Expansion of precision medicine, where imaging data is analyzed alongside genomics, pathology, and EHR data.
- Cross-border care delivery, as medical tourism and international collaborations expand.
Imaging will no longer be a “support service” in hospitals but a strategic pillar of healthcare delivery, shaping not just diagnoses, but organizational direction and sustainability.
Imaging as a Hospital-Wide Asset
Once integrated, imaging ceases to be a departmental tool and becomes a hospital-wide strategic asset.
- For care delivery: It underpins emergency, surgical, oncology, and chronic disease care.
- For administration: It drives cost control, performance metrics, and revenue assurance.
- For future growth: It lays the foundation for advanced registries, clinical research, and population health planning.
Hospitals that fail to integrate risk being left behind — with fragmented workflows, compliance gaps, and dissatisfied patients.
Every hospital has its own realities — from patient volumes and regulatory requirements to specialty-specific workflows. The best way to understand how a Hospital Management System (HMS) with PACS integration can fit into your environment is to see it in action.
A tailored demo will allow your team to:
- Explore how imaging and clinical workflows come together in a single system.
- See how administrators can track utilization, turnaround times, and financial performance.
- Understand how physicians and nurses can access patient data and imaging at the point of care — without toggling between systems.
- Evaluate interoperability with existing tools, from billing to national health insurance schemes.
Take the next step: Request a live demonstration with our specialists. In under an hour, your leadership team will gain clarity on how enterprise imaging intelligence and hospital-wide integration can improve care delivery, reduce costs, and prepare your facility for the future of healthcare.