A Cross-Functional Reality Check Across Clinical, Billing, and IT Functions
Hospitals rarely initiate a review of their Hospital Management System (HMS) in the absence of substantive operational considerations. Persistent inefficiencies within clinical workflows, prolonged billing and reconciliation cycles, increasing regulatory and compliance requirements, and limitations in enterprise reporting or scalability often compel senior management to reassess whether the existing system continues to adequately support institutional objectives.
Despite such clarity of intent, a considerable proportion of HMS initiatives encounter difficulties during evaluation, implementation, or post–go-live stabilization. In these situations, the system itself is frequently identified as the principal cause. In practice, however, the more prevalent issue is a lack of organizational readiness.
HMS readiness is not defined by dissatisfaction with an existing platform. It is defined by the extent to which a hospital, as an operating institution, is prepared to absorb and sustain structural change across clinical operations, financial processes, and information technology governance simultaneously. Where such readiness does not exist across functions, even technically robust systems struggle to deliver durable value.
The blog examines HMS readiness as a cross-functional institutional condition—one that warrants deliberate consideration prior to the commencement of vendor evaluations, system demonstrations, or implementation planning.
Why HMS Readiness Is Commonly Overestimated
Within many hospitals, readiness is assumed rather than formally assessed. Indicators such as clinician dissatisfaction, billing backlogs, or increasing dependence on manual interventions are often interpreted as evidence that the organization is prepared for a system change.
These indicators, however, reflect operational pressure rather than preparedness.
An HMS transition introduces fundamental changes to documentation practices, revenue capture logic, reporting structures, system integrations, and governance models. Where underlying processes are fragmented, insufficiently documented, or inconsistently applied, the introduction of a new system does not resolve these deficiencies. Instead, it exposes them more visibly and embeds them more permanently.
Hospitals that manage HMS transitions with greater stability typically adopt a different sequencing. Rather than beginning with system features or vendor comparisons, they first evaluate internal readiness across clinical, billing, and IT functions. This enables technology decisions to be grounded in institutional reality rather than driven solely by urgency.
Clinical Readiness: Institutional Consistency Prior to System Enablement
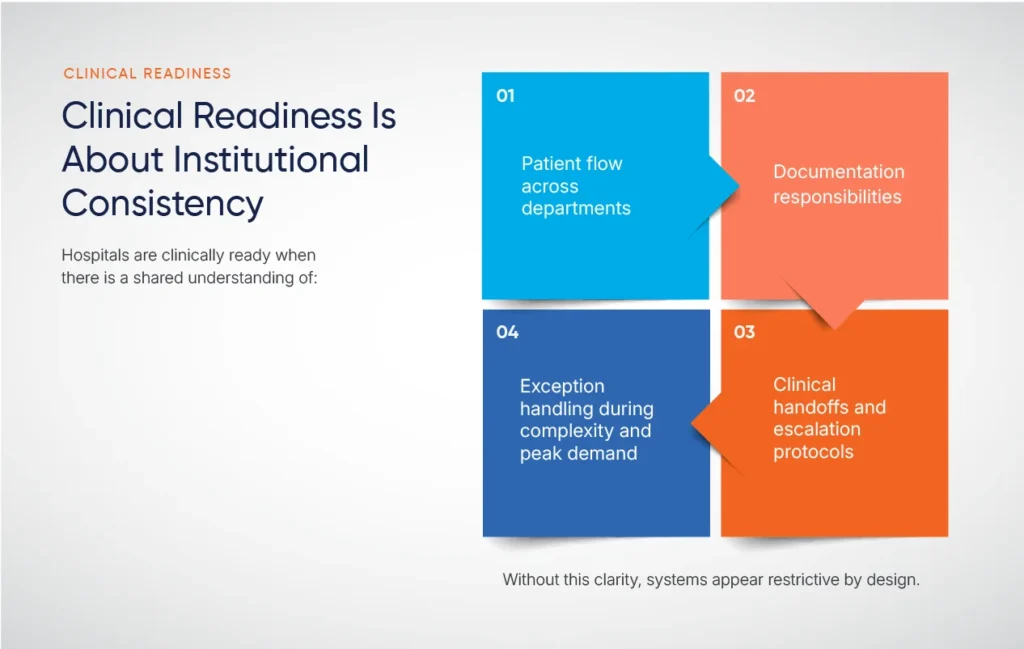
Clinical readiness is frequently assessed through measures of user acceptance or digital familiarity. While relevant, these measures are not reliable indicators of preparedness for an HMS transition.
True clinical readiness is predicated on process consistency at an institutional level.
Hospitals that demonstrate clinical readiness possess a shared and operationally grounded understanding of how care is delivered across departments and services. This includes clarity regarding patient flow, documentation responsibilities, clinical handoffs, escalation protocols, and the management of exceptions during periods of peak demand or clinical complexity.
In the absence of such clarity, HMS configuration efforts become attempts to formalize informal practices. This frequently results in systems being perceived as restrictive or misaligned—not due to inherent system limitations, but because unresolved variability has been embedded into the system design.
Clinical readiness is also contingent upon governance maturity. Institutions with clearly defined decision-making structures for clinical standards, documentation policies, and change control are better positioned to make coherent configuration decisions. Where governance is fragmented or ambiguous, HMS initiatives often devolve into prolonged negotiations rather than structured transformation programs.
Finally, clinical readiness reflects an organization’s capacity to absorb change. Hospitals with a demonstrated history of implementing clinical protocols, regulatory updates, or operational reforms tend to adapt more effectively to HMS-driven transformation. Where such initiatives have historically encountered resistance, similar challenges frequently re-emerge during system adoption.
Billing Readiness: Structural Discipline Beyond Transactional Continuity
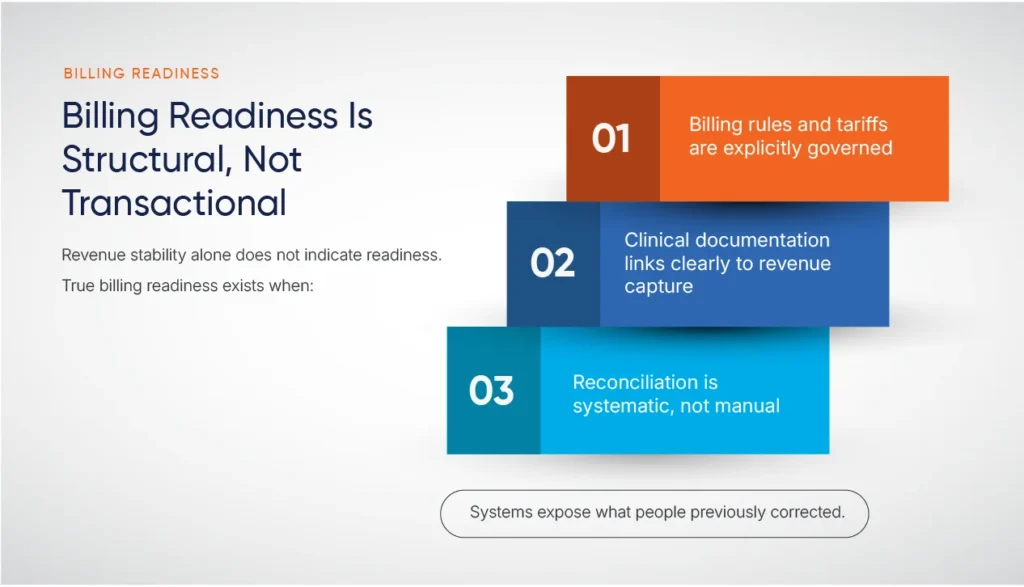
Billing and finance functions play a central role in HMS initiatives, yet billing readiness is often assessed superficially. Continued revenue inflow is frequently interpreted as evidence of operational stability.
HMS transitions, however, subject billing structures to a level of rigor that routine operations do not.
Billing readiness is defined by the degree to which billing logic is explicit, governed, and resilient to systemic change. Hospitals that exhibit billing readiness typically demonstrate:
- Clearly articulated billing rules, tariffs, and exception-handling mechanisms
- Defined dependencies between clinical documentation and revenue capture processes
- Established reconciliation practices that systematically identify delays, denials, and revenue leakage
Organizations that rely extensively on manual intervention or individual expertise to resolve billing exceptions often experience disruption during HMS transitions. Processes previously corrected through informal effort become constrained by system logic, exposing structural gaps that were not previously apparent.
Financial transparency is a further indicator of readiness. Hospitals capable of clearly articulating revenue cycle performance across payers, service lines, and timeframes are better positioned to evaluate the impact of system change. In the absence of such baseline visibility, post-implementation performance is difficult to assess objectively.
Billing readiness also encompasses regulatory adaptability. As payer frameworks and compliance requirements evolve, the HMS must accommodate change without disproportionate reconfiguration. Hospitals that conceptualize billing as a structured system, rather than a series of tasks, make more sustainable technology decisions.
IT Readiness: Governance and Accountability Beyond Infrastructure

IT readiness is frequently defined in terms of infrastructure availability and security posture. While foundational, these elements do not capture the full scope of preparedness required for an HMS transition.
Effective IT readiness is characterized by governance and ownership.
Hospitals that are IT-ready for an HMS review typically demonstrate:
- Clear internal accountability for integrations, data governance, and vendor coordination
- A comprehensive understanding of existing system dependencies and interoperability requirements
- Experience managing enterprise system change with internal decision-making authority
In environments where IT functions primarily as a support service, HMS transitions often become reactive. Integration challenges surface late, data migration risks are underestimated, and implementation timelines are extended.
Data maturity represents an additional dimension of readiness. This includes clarity regarding data sources, data quality, migration scope, and reporting continuity. Treating data migration as a purely technical exercise frequently results in operational disruption following go-live, particularly in financial reconciliation and historical reporting.
IT readiness further requires realistic resource and capacity planning. HMS initiatives demand sustained engagement over extended periods. Organizations that fail to realign priorities or allocate appropriate resources risk execution fatigue and compromised outcomes.
Cross-Functional Alignment: The Critical Determinant of Outcomes
The most common cause of HMS underperformance is not functional inadequacy, but misalignment across functions.
- Clinical teams prioritize operational flexibility.
- Billing teams emphasize control and accuracy.
- IT teams focus on standardization and risk mitigation.
Each perspective is legitimate. Challenges arise when these priorities are not reconciled at an institutional level.
True readiness exists when trade-offs are explicitly acknowledged and resolved. Clinical documentation standards must reflect billing and compliance requirements. Billing controls must accommodate clinical realities. IT architectures must balance standardization with operational necessity.
Absent such alignment, HMS decisions tend to optimize one function at the expense of others. The resulting friction is often attributed to system limitations rather than unresolved organizational choices.
Leadership Readiness: The Defining Variable
Even where functional readiness is present, HMS initiatives frequently falter in the absence of leadership readiness.
Leadership readiness is reflected in clarity of purpose and accountability. This includes a shared understanding of the rationale for the HMS review, clear definitions of success beyond implementation, and established mechanisms for resolving cross-functional conflicts.
Hospitals that approach HMS reviews primarily as procurement exercises often delegate critical decisions without sustained oversight. In contrast, organizations that recognize HMS initiatives as enterprise-level change programs maintain consistent leadership engagement throughout the lifecycle.
Timeline discipline constitutes a further indicator. Unrealistic schedules imposed without regard to operational capacity frequently lead to compromises that manifest later as adoption, quality, or compliance issues.
Leadership readiness also involves articulating guiding principles. Clear positions on standardization, customization, scalability, and long-term system governance provide a consistent framework for decision-making across the organization.
Evaluating Readiness Prior to System Commitment
Assessing HMS readiness does not imply deferring decisions indefinitely. Rather, it ensures that decisions are informed by institutional constraints and capabilities.
Hospitals that invest time in evaluating readiness across clinical, billing, and IT functions consistently experience:
- More focused and relevant vendor evaluations
- Higher-quality internal discussions during demonstrations and workshops
- Clearer scoping and configuration decisions
- Smoother transitions with fewer post–go-live corrective cycles
Most importantly, such institutions avoid conflating urgency with preparedness.
Readiness as an Institutional Capability
HMS readiness is not a one-time assessment associated with a specific system review. It is an institutional capability that reflects organizational maturity.
Hospitals that cultivate the discipline to evaluate readiness objectively—across functions rather than in isolation—develop greater resilience. They are better positioned to absorb change, align systems with care delivery models, and make technology investments that support long-term strategic objectives.
Before determining whether a new HMS is the appropriate solution, senior leadership should first consider a more fundamental question:
Is the organization prepared for the level of operational and structural change that an HMS transition will introduce?
The answer to this question frequently determines whether the next HMS becomes a foundation for sustainable improvement—or another system constrained by unresolved institutional challenges.
Moving the Conversation Forward
Hospitals that are reflecting on a potential Hospital Management System review often find value in early, consultative discussions that help surface cross-functional alignment considerations, governance implications, and institutional readiness—prior to initiating any formal evaluation process.
In this context, we wanted to share the above perspective as a reference, should it be useful to your leadership team as you consider HMS-related priorities. Many institutions find that a brief, informal discussion at this stage helps clarify internal considerations before progressing further.
If such a conversation would be helpful, we would be pleased to coordinate a short exploratory discussion at a time convenient to your team. The intent would be solely to support institutional clarity, without any obligation toward a formal evaluation or next step.

